Almost everyone has heard of varicose veins. In most people, this vascular disease is associated with foot problems, but often the pelvic organs become the site of localization of the pathological process. One type of this pathology is varicose veins of the uterus.
The disease is diagnosed primarily in women or girls of childbearing age, but in some cases it also develops in adolescent girls. In order to cope with the pathology, it is important to know the main causes and symptoms of its occurrence and to know the methods of treatment.
Characteristics of pathology
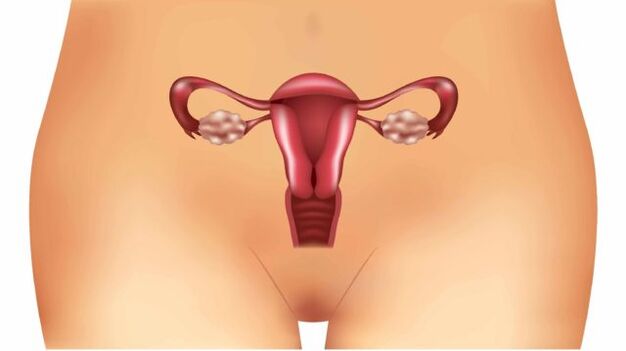
Uterus returns, what is it? This medical term refers to a disease caused by a number of pathological factors affecting the venous network of the pelvic organs:
- Thinning of the vessel walls.
- Formation of vascular nodules.
- Dilation of the venous lumen.
These three factors negatively affect the process of blood circulation in a separate part of the organ and lead to valvular insufficiency of the veins in the same area. The disease is difficult to diagnose due to the lack of obvious clinical symptoms and similarity to diseases of the pelvic organs of an inflammatory nature. For these reasons, the pathology is often detected at severe stages when treatment is much more complicated.
Gynecologists distinguish two subtypes of the pathological process:
- Uterine varicose veins.
- Varicose veins of the cervix.
In any case, because of the dangerous complications of the disease, which include inflammatory processes that cover the uterus, ovaries, and vagina. The most serious complication is infertility.
Causes of the disease
Understanding the factors behind the development of the disease has a number of key benefits. First, it allows the physician to diagnose faster and more accurately, as well as prescribe appropriate treatment. Second, a woman will be able to prevent the pathology from developing.
Consider the most likely causes of uterine varicose veins:
- Pregnancy is a major factor in the development of the pathological process. Already at the embryonic stage, and then with the growth and development of the fetus, uterine circulation increases (much depends on the period). However, in vessels with a weakened venous wall, the operation of the valves is disturbed and prolonged. In addition, a growing fetus increases the load on the pelvic organs, which can also give impetus to the development of the disease.
- Long-term use of hormonal drugs. Each drug adversely affects the condition of the vessels, their walls lose their elasticity.
- Another factor that provokes the disease is a decrease in motor activity. A sedentary or sedentary lifestyle will lead to a decrease in muscle contraction function, resulting in impaired blood circulation.
- Increased physical activity in the pelvic region. In this case, as during pregnancy, the blood flow to the pelvic organs, especially the uterus, increases.
- Increased constipation - in this case, the cause of varicose veins will again be an increase in blood flow. However, due to increased intra-abdominal pressure, circulation is now increased.
- Congenital anomalies in uterine structure.
- Artificial termination of pregnancy.
- Difficult childbirth.
- Inflammatory processes in the pelvic organs.
Symptoms and diagnosis
The complexity of diagnosing uterine varicose veins lies in the fact that the symptoms of this disease are masked by other pathologies. In addition, the clinical picture of the disease is rather poor:
- Frequent pain in the lower abdomen, more than 3-4 times a week, closer to the vulva. The pain syndrome is pronounced, the nature of the pain is pulling and sore. In some cases, the pain is so severe that the woman loses her ability to work, even getting out of bed.
- More than 80% of women with uterine varicose veins experience discomfort or even pain during or after intercourse.
- Violation of the menstrual cycle, delayed menstruation for 50-60 days is possible. In this case, the discharge is often small, the duration of menstruation is 5-7 days. For many women, prolonged lack of menstruation is the first sign of menopause.
This clinical picture is inherent in many other gynecological diseases. For this reason, it is not possible to make a diagnosis based on symptoms alone, the doctor must prescribe a number of diagnostic measures. In addition, the symptoms in the cervical vein are roughly the same.
Important: Uterine varicose veins are mainly diagnosed in the second stage, as this is when the symptoms described begin to bother the woman. The sooner the pathology is detected and treatment begins, the less likely it is to have complications, especially infertility.
As for directly assigned studies, the following are:
- Ultrasound performed by the transvaginal method.
- CT of pelvic organs.
- Dopplerography.
- Selective ovaricography.
The need for each diagnostic method depends on the data obtained as a result of the ultrasound, as it is performed first.
Characteristics of the disease during pregnancy
Due to the increased load on the whole body and the pelvic organs, the chances of developing uterine varicose veins increase during pregnancy. Until a woman gives birth, the disease cannot be treated.

The pathology that develops during pregnancy influences the choice of mode of transport. Very often, the doctor decides to have a cesarean section. This includes thrombophlebitis, internal bleeding, thrombosis, etc. to avoid complications in the form of
Regardless of the time during which the disease was diagnosed, the woman should be monitored regularly by a doctor to monitor the condition of the fetus and the progression of varicose veins.
Important: When planning a pregnancy, perform a test to identify uterine varicose veins and other gynecological problems. This helps to avoid complications during childbirth and reduces the risk of fetal developmental pathologies.
Treatment of the disease
To get professional help with varicose veins, you need to see a doctor, initially a gynecologist, who will then refer you to a phlebologist.
The treatment is based on drug therapy, which consists of taking the following drugs:
- Venotonics - drugs in this group have a beneficial effect on the condition of blood vessels. They tone capillaries and blood vessels, reduce their permeability, increase flexibility and strengthen the walls of veins.
- Drugs that reduce the viscosity of the blood - contribute to the general improvement of blood inflow and outflow in the affected vessels, reduce the likelihood of thrombosis. The devices in this group are contraindicated in cardiac pathologies.
Important: Any medication should only be prescribed by a doctor, taking into account the preliminary diagnosis, the patient's medical history and the stage of development of the disease. It is important to pay special attention to the women in the position.
Treatment methods
In addition to drug therapy for full treatment, it is important to implement an integrated approach and the following recommendations:
- adherence to sleep patterns;
- minimizing physical activity while maintaining mobility;
- following a diet rich in vegetables, fruits and vitamin E-rich oils;
- supportive sports, physiotherapy;
- complete exclusion of bad habits;
- some doctors recommend performing Kegel exercises that strengthen the vaginal muscles.
Surgical intervention
Such drastic measures are needed in cases where conservative treatment has not produced adequate results or the disease has been detected at a late stage. The following surgical procedures are the most popular:
- Phlebectomy is the removal of certain sections of small blood vessels.
- Laser coagulation is the most economical way to restore normal blood flow.
- Sclerotherapy is the introduction of an agent into a cavity in a vein that helps it to stick to it. Lack of blood supply in the vessel leads to spontaneous elimination.
- In the most severe cases, complete removal of the uterus should be performed, sometimes with appendages.
ethnology
Alternative methods are one option for complex treatment in a conservative manner. They are not a complete substitute for drug therapy, but they can generally affect the success of therapy.
The most effective tools in traditional medicine are:
- Horse chestnut infusion: take 100 grams of chestnut fruit, chop with the peel. Pour the resulting raw material with enough vodka to cover the crushed fruit with 4-5 millimeters. Stick in a dark place for 14-15 days. Thereafter, the infusion should be taken 10 drops twice a day. The device strengthens blood vessel walls and dilutes blood.
- Purple tincture: For 0, 5 liters of vodka take 100 grams of purple flowers and 30 grams of propolis. All ingredients are poured with vodka and left in a dark place for 30 days (shake every 2-3 days). The tincture is then filtered and 15 ml is consumed three times daily before meals.
Remember to consult your doctor before using even the most innocuous traditional medicine.
Complications of the disease
In the absence of proper treatment, they can be dangerous due to complications of uterine varicose veins. These complications include:
- internal bleeding;
- thrombosis;
- inflammatory processes of the genitals;
- menstrual disorders;
- hormonal dysfunction of the ovaries;
- infertility.
Preventive measures
It is always better to prevent the development of a disease than to deal with it or its consequences later. To prevent uterine varicose veins, follow these simple rules:
- to lead an active lifestyle, to walk and walk more;
- to exercise;
- eat healthy food, less fatty, fried, spicy, spicy, sour;
- visit your gynecologist regularly, especially for the slightest complaint.

Despite the difficulty in detecting varicose veins in your uterus, contact your doctor if you experience any of the symptoms described above to prevent the disease from progressing and complicating it. It is also important to note that self-medication in such cases is contraindicated, with careful diagnosis and constant monitoring by a gynecologist and phlebologist.












































